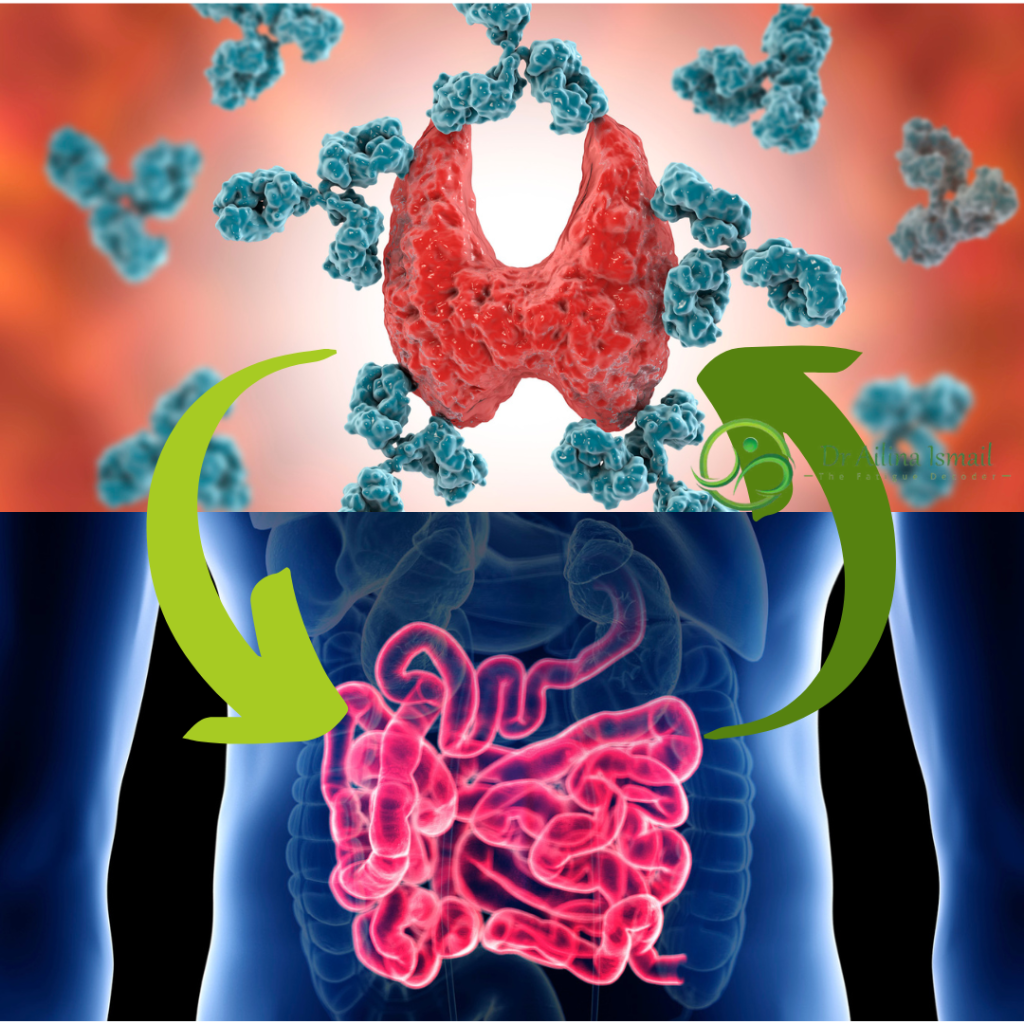
The gut has long been recognized as a powerhouse of health, playing a pivotal role in our overall well-being. But did you know that it also holds the key to understanding autoimmune disorders like Hashimoto’s thyroiditis? In this article, we’ll explore the intricate relationship between the gut and the immune system, and how disruptions in gut health can contribute to autoimmune conditions.
The Gut-Immune Axis:
Our gut is home to trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in maintaining a balanced immune response. The gut microbiota interact closely with the immune system, influencing its development, function, and response to threats. This dynamic relationship forms the gut-immune axis, a complex network that regulates immune activity throughout the body.
Autoimmune Disorders and the Gut:
In autoimmune disorders like Hashimoto’s thyroiditis, the immune system mistakenly attacks the body’s own tissues, in this case, the thyroid gland. While the exact cause of autoimmune diseases remains elusive, growing evidence suggests that disturbances in gut health may play a significant role in triggering and exacerbating these conditions.
Leaky Gut Syndrome:
One such disturbance is leaky gut syndrome, a condition characterized by increased intestinal permeability. In leaky gut syndrome, the tight junctions between intestinal cells become compromised, allowing undigested food particles, toxins, and pathogens to leak into the bloodstream. This influx of foreign invaders triggers an immune response, leading to inflammation and potential autoimmune reactions.
Dysbiosis:
Another factor implicated in autoimmune disorders is dysbiosis, an imbalance in the gut microbiota composition. Dysbiosis can arise from various factors, including diet, stress, medications, and environmental toxins. When the delicate balance of beneficial and harmful bacteria in the gut is disrupted, it can impair immune regulation and promote inflammation, paving the way for autoimmune processes.
The Role of Molecular Mimicry:
Molecular mimicry is a phenomenon in which microbial or dietary proteins bear resemblance to host tissues. When the immune system mounts an attack against these foreign proteins, it may inadvertently target similar proteins found in our own tissues, leading to autoimmune reactions. In the case of Hashimoto’s thyroiditis, molecular mimicry between bacterial or dietary proteins and thyroid antigens may contribute to the development of autoimmunity.
Healing the Gut to Heal the Body:
The good news is that by addressing gut health, we can potentially mitigate autoimmune processes and improve overall wellness. Strategies for promoting gut health include:
- Diet: Adopting a nutrient-dense, anti-inflammatory diet rich in whole foods, fiber, and fermented foods can nourish the gut microbiota and reduce inflammation.
- Gut-Healing Supplements: Targeted supplements such as probiotics, prebiotics, digestive enzymes, and gut-repairing nutrients like L-glutamine and collagen can support gut integrity and microbial balance.
- Stress Management: Practicing stress-reducing techniques such as mindfulness, meditation, and yoga can help modulate the gut-brain axis and promote gut health.
- Lifestyle Modifications: Avoiding environmental toxins, optimizing sleep, and staying physically active are essential for maintaining gut health and supporting immune function.
In the complex interplay between the gut and the immune system lies the key to understanding and managing autoimmune disorders like Hashimoto’s thyroiditis. By prioritizing gut health through diet, lifestyle, and targeted interventions, we can potentially mitigate autoimmune processes, alleviate symptoms, and embark on a path to lasting wellness. Remember, a healthy gut is the foundation of a healthy body, and nurturing it is paramount in the journey towards optimal health and vitality.